Vaccination and Drugs
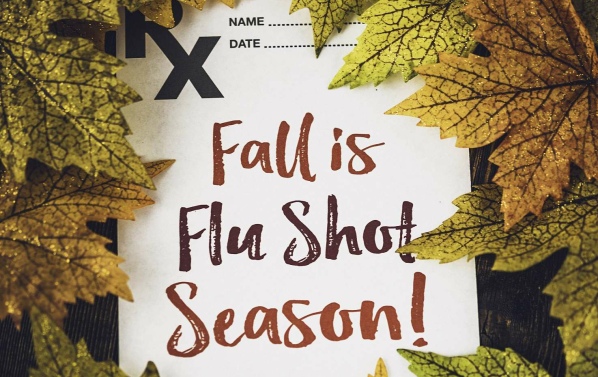
CDC Predicted “Second Wave” of Influenza This Year
AN ARTICLE PUBLISHED BY RISHMA PARPIA AND THE NATIONAL VACCINE INFORMATION CENTER.
Although spring is when the typical “flu season” ends, officials at the U.S. Centers for Disease Control and Prevention (CDC) warned in mid-March 2018 that a “second wave” of influenza B virus appeared to be on the way and could cause more illness, especially among young children.[1] [2] [3] News reports stated that the majority of the 2017-2018 flu season was dominated by the H3N2 virus, an influenza A strain, while the second wave would be dominated by the influenza B strain.[3] According to the CDC’s weekly surveillance report, for the week ending March 17, 2018, total influenza cases were declining but there were more laboratory confirmed cases of influenza B viruses than influenza A viruses.[4]
According to CDC’s spokeswoman Kristen Norlund, “B is usually worse for younger children. We often see an increase in influenza B cases during seasons when influenza A/H3N2 was the predominant virus earlier in the season.”2 Gary Leonardi, PhD, a virologist at Nassau University Medical Center in New York added that, “There has certainly been diminished influenza activity in the past three weeks. However, influenza is still circulating.”[2]
According to CDC officials, previously contracting influenza A strain virus does not provide immunity against B strain viruses. In March, health officials continued to warn that it is still not too late to get a flu shot, even though this year’s flu shot was estimated to be only about 25 percent effective for type A and about 42 percent effective for type B influenza.[2] TIME Magazine reported that, “The CDC recommends vaccination “as long as flu viruses are circulating”—and with 17 states still reporting widespread flu activity, that puts us squarely within that window.”[3]
“Flu Season” is Over So Why a Second Wave?
There is a general consensus that influenza outbreaks generally occur during the fall and winter months, beginning late November through March.5 While there are many theories circulating about why influenza outbreaks occur in the winter, the answer to why it is predominantly a winter illness is not full understood.[6]
One of the theories is that the influenza virus is more stable and lingers in the air a lot longer when the air is cold and dry.[7] Currently, it is spring, past the typical “flu season”, yet the CDC predicted there would be a second wave of influenza B. How is this possible?
The fact is that influenza viruses are detected all year round in the United States, not just during what is called the “flu season”.[8] It is very possible to get infected with influenza virus during the spring and summer months, as well.[9] The question that needs to be answered is: Why do is it that some people get seriously ill with influenza and have complications that lead to hospitalizations and even death, while others do not?
Susceptibility Versus Exposure
Contracting influenza is not a random occurrence.[10] Logically, if exposure to the influenza virus, which is already in the environment, were the one and only factor determining whether a person gets sick, then everyone would get sick each time they came into contact with the influenza virus.[10] For example, in situations where people are exposed to the virus in closed environments, not everyone will get sick. The point is that it is not only exposure to the influenza virus that determines whether a person gets sick, but individual susceptibility also plays a crucial role.[10]
According to a study published in PLOS Genetics, “Exposure to influenza viruses is necessary, but not sufficient, for healthy human hosts to develop symptomatic illness. The host response is an important determinant of disease progression.”[11] The study conducted by researchers at the University of Michigan is the first study of this kind whereby seventeen human volunteers received intranasal inoculation of influenza H3N2.[11] Nine of these volunteers developed mild to severe symptoms. The remaining volunteers did not notice any symptoms.[11]
Alfred Hero, PhD, a professor at University of Michigan’s College of Engineering and an author of the study states, “Many people might conclude that if you are exposed to a virus and you don’t get sick, it’s because the virus didn’t stick or it was so weak, it just passed right through your system and your system didn’t notice. That’s not a correct notion.”[12]
Dr. Hero adds:
There is an active immune response which accounts for the resistance of certain people getting sick, and that response is just as active as the response we all know and hate, which is being sick with the sniffles, fever, coughing and sneezing. It’s just that the responses are different. There is a behind the scene active immune response even when you don’t get sick. What we found were differences in their biological metabolism and gene expression. These differences had to do with antioxidants.[12]
Dr. Hero says that “drinking juice, and eating fresh fruits and vegetables to load up on antioxidants may be the answer to avoid getting sick with the flu.”[12]
Public health officials are quick to promote the influenza vaccine but fail to inform the public that susceptibility to getting sick with an influenza infection is also associated with poor nutrition, increased stress levels, sleep deprivation and a vitamin D deficiency. Given what is known about how the body’s immune system works, it makes sense to consume nutritious, wholesome foods, manage stress levels, get adequate sleep and the right amount of vitamin D all year round to help protect against getting seriously ill from influenza or any other infectious disease.
References:
[1] Seiger T. CDC Warns of Second Wave of Flu Virus. Wsbtv Mar. 30, 2018.
[2] Ricks D. Flu is Not Done: B Strains Dominate Season’s Second Wave. Newsday Mar. 29, 2018.
[3] Ducharme J. A Second Wave of Flu May Be on the Way. TIME Mar. 27, 2018.
[4] U.S Centers for Disease Control and Prevention. Weekly U.S Influenza Surveillance Report. CDC.gov Mar. 30, 2018.
[5] CDC. Current and Past Flu Seasons. CDC.gov Mar. 22, 2018.
[6] Niall HD. Why do we get the flu most often in the winter? Are viruses more virulent in cold weather? Scientific American.
[7] Kolata G. Study Shows Why Flu Likes Winter. The New York Times Dec. 5, 2007.
[8] CDC. The Flu Season. CDC.gov July 26, 2016.
[9] Duda K. Can You Get the Flu in the Summer? Very Well Health Nov. 24, 2017.
[10] What Doctors Don’t Tell You: Colds and Flu: Keeping Well in the Winter Season. Healthy.net.
[11] Huang Y, Zaas A, Rao A, et al. Temporal Dynamics of Host Molecular Responses Differentiate Symptomatic and Asymptomatic Influenza A Infection. PLOS Genetics 2011
[12] Taylor K. Why Some People Don’t Get the Flu. NBC News Aug. 30, 2011.